Lupus anticoagulant—proficiency test and preanalytics
-
Lupus anticoagulant—proficiency test and preanalytics
in 2024 issues, ARTICLES, Coagulation, IN THIS MONTH’S ISSUE, March 2024, May 2024, MAY 2024
https://www.captodayonline.com/lupus-an … analytics/Geoffrey Wool, MD, PhD
Nicole Dodge Zantek, MD, PhD
Marian Rollins-Raval, MD, MPHWhat is a lupus anticoagulant (LA)? LA is somewhat of a misnomer. Many patients with this condition do not have systemic lupus erythematosus (SLE) and usually do not bleed. However, the in vitro phenomenon was originally described in patients with SLE, as well as other autoimmune disorders—thus use of the term “lupus,” and this does often lead to prolonged in vitro coagulation testing—thus use of the term “anticoagulant.” Ultimately, antiphospholipid antibodies were identified as the causative factor for positive LA testing.1 These antiphospholipid antibodies may or may not have identifiable specificity for selected phospholipid-binding proteins by currently available immunoassays. Clinically, these antiphospholipid antibodies have been associated with increased risk of thrombosis and pregnancy morbidity, which together with the laboratory criteria define antiphospholipid syndrome.
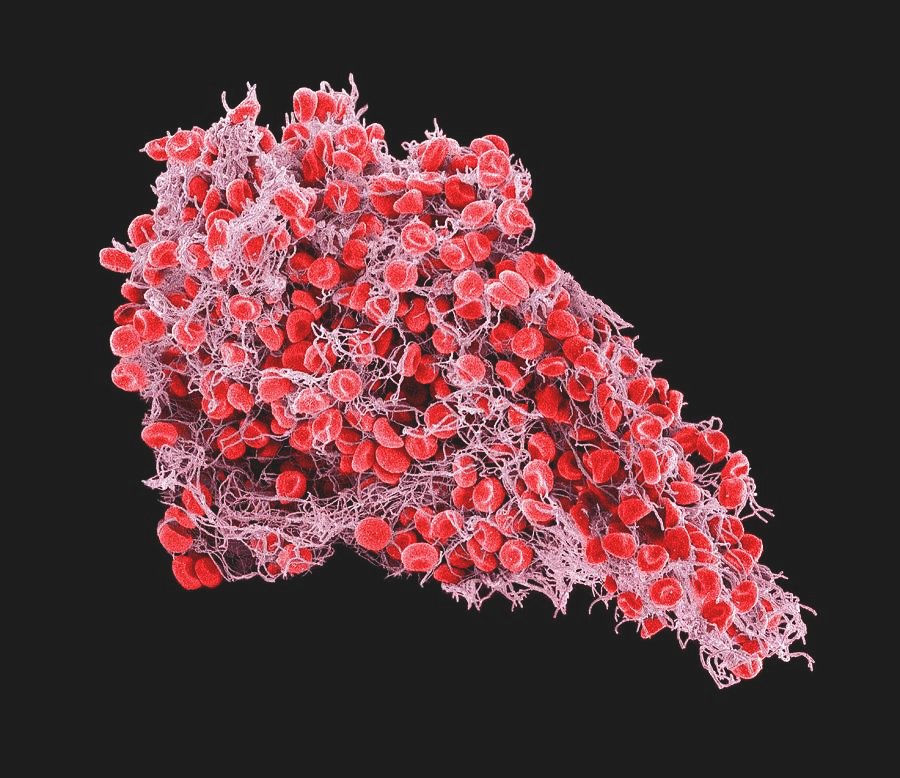
LA testing is achieved by demonstrating phospholipid dependence using a paired-assay system (e.g. screen step and confirm step). An LA is positive when a screening clot-based assay shortens significantly with the addition of supplementary phospholipid in the confirm step. The theory behind this is that the additional phospholipid will neutralize some of the antiphospholipid antibodies, allowing the clotting reaction to progress more quickly. Many routine coagulation assays for activated partial thromboplastin time (aPTT) and prothrombin time (PT) are “lupus insensitive” with high amounts of phospholipid in the reagent, so as not to show LA interference when that is not the desired target of laboratory testing. For patients for whom clinical suspicion for an LA exists, more appropriate LA-sensitive assays are available.
Many of these assays are commercially available and Food and Drug Administration approved or cleared, if used according to the manufacturers’ instructions for use. They consist of paired tests: a “screening” step with “low” phospholipid reagents and a “confirmatory” step with “high” phospholipid reagents. The results of these paired assays may be reported as screen to confirm ratio (Fig. 1) or a change in seconds (Fig. 2) to define positivity. Many commercial and laboratory-developed assays integrate heparin neutralization, normal plasma mixing components, and/or standardization with normal donors/normal pooled plasma into the reagent sets to minimize the effects of heparin contamination, patient clotting factor level variation, or differences in reagents. Most guidelines recommend two different methods—dilute Russell Viper Venom Time (dRVVT) and aPTT, for example—because no single assay can detect all LA.2,3 All assays have limitations, which may impact all or some reagents or methods, making LA testing challenging to perform and interpret.
CAP LA proficiency testing.
The CAP CGS1 proficiency testing Survey provides a twice yearly challenge for laboratories that perform LA testing. More than 350 laboratories participate in this Survey. The CAP Hemostasis and Thrombosis Committee decided in 2022 to update the CGS1 Survey reporting form. The form had previously not been changed in many years despite multiple additional reagents having become available on the market and updates to international guidance on LA testing, interpretation, and reporting.In the past, the form had divided LA testing reporting into two categories: dRVVT-based testing and all other LA testing. Laboratories primarily reported aPTT-based testing in the “all other LA testing” category, but the category would also include any alternative methods (e.g. dilute prothrombin time or taipan/ecarin time testing). Additionally, the aPTT-based testing reporting was not divided by reagent type or manufacturer (that is, common commercially available aPTT-based kits were not differentiated, nor were less commonly used techniques such as platelet neutralization procedure). The “all other LA testing” category also captured no quantitative data; it captured only if the screening clotting time was normal/prolonged and if the system showed the presence of an LA or not. Finally, the form had duplicative areas for a summative assessment of the presence of an LA in the sample that were not clearly labeled.
The CAP Hemostasis and Thrombosis Committee also noted that the form was confusing, leading some laboratories to report LA reagents in the incorrect section of the form. For instance, dRVVT reagent results were being reported as an LA-sensitive aPTT. Routine LA-insensitive aPTT reagent results were also being reported as an LA-sensitive aPTT.
The LA portions of the CGS1 Survey had not previously been graded, and one of the goals of the form updates was to allow the LA final interpretation response to be graded. Additionally, capturing more granular data with correct categorization is helpful for laboratories looking to implement or change their LA testing, as they are able to directly compare reagent usage and performance. Improved data quality is also helpful to the broader hemostasis community by making it possible for potential publications of LA proficiency testing results to be more insightful and meaningful. The new, more granular data capture will also provide information regarding practice patterns and testing algorithms across different laboratories for this nonstandardized and complex type of testing.
CGS1-A-2023 was the first Survey with an updated reporting form. Our goal was to streamline and separate reporting of dRVVT-based LA testing and aPTT-based LA testing, and to separate any other remaining LA methods into their own category. We also began capturing granular data on screen, mix, confirm, and ratios for each of the LA reagent categories.
The form updates used for CGS1-A-2023 generated numerous inquiries from Survey participants. LA testing is complex, and designing a form to match all users’ processes posed significant complexities. The form was further improved for CGS1-B-2023, and fewer inquiries were received.
LA testing has historically followed a screen-mix-confirm paradigm. As reagent kit packages have become more popular, this paradigm has changed. In addition, current guidelines differ in when and how mixing studies should be used in the diagnostic algorithm and which interpretation should be used to determine correction (that is, mixing-test specific cutoff versus calculation of the index of circulating anticoagulant). FDA-approved LA reagent packages contain both a low phospholipid and high phospholipid reagent; a separate mixing study is often not required in this setting and some reagents include pooled normal plasma (all testing is therefore performed on a mixed sample). Some laboratories found the new form to be confusing for the following reasons: 1) the form had an entry for reporting a mix for the aPTT-based system, but they might not perform a mix in that system; 2) the form had fields for screen and confirm results for the aPTT-based system, but the laboratory staff did not know which kit reagent was being referred to by the “screen” and “confirm” nomenclature; or 3) the lab might perform a screening LA-sensitive aPTT as well as an aPTT-based kit that has low and high phospholipid reagents. In response to No. 3, the committee created two fields within the confirmatory area of the LA-sensitive aPTT section, one for low phospholipid and one for high phospholipid reagents.
Preanalytics in LA testing.
Beyond the analytic phase of testing evaluated by CGS1, LA is further complicated by multiple preanalytical factors that can lead to false-positive and false-negative results and thus ultimately to inappropriate clinical decisions. Appropriate timing of testing and consideration for the potential impact on results is paramount. Several studies have shown a high rate of inappropriate timing of thrombophilia testing, including antiphospholipid antibody testing.4,5Great care should be taken to ensure the specimen is of the highest quality with clean venipuncture, sufficient centrifugation to remove platelets, and proper aliquoting and storage.2,3 Testing during the acute phase of illness, such as in a hospital admission, can be associated with false-negative and false-positive results.6,7 Elevated levels of fibrinogen and factor VIII can lead to decreased clotting times resulting in a false-negative.8 Elevated C-reactive protein can lead to positive LA results with some aPTT assays, so testing in the setting of infections, inflammatory states, and immune conditions can result in false-positive results.9 The setting of acute thrombosis can also lead to consumption of antiphospholipid antibodies in a clot, potentially leading to false-negative results.
Numerous studies have confirmed that anticoagulants may cause false-positive LA results; however, it should also be appreciated that false-negative LA can occur.10 While LA screening clotting times, such as the aPTT or dRVVT, may be elevated on anticoagulation, the next steps in testing (mixing studies and phospholipid-dependent confirmatory tests) may give variable responses leading to alternative interpretations of LA present (mix+, confirm+), non-LA inhibitor present (mix+, confirm−), and a potentially inconclusive pattern (mix−, confirm+) in a patient who otherwise does not have an LA. This may lead to additional testing and inappropriate clinical decisions, supporting that LA testing should not be performed while on anticoagulants.11,12 Strategies to consider when testing a patient on anticoagulation include mixing of the patient plasma with pooled normal plasma, use of integrated assays compared with the three-step procedure, use of test procedures less affected by anticoagulants, use of antidotes or neutralizers to quench anticoagulant activity, collection of patient specimens at the expected treatment trough, and temporary discontinuation of anticoagulation.10,12,13 The Food and Drug Administration has not cleared most of these methods and/or reagents.
The patient presenting in the acute setting with a new thrombosis and need for anticoagulation creates a dilemma for clinicians. It is desirable to delay testing until the patient has completed treatment for venous thromboembolism. However, clinicians may be concerned about antiphospholipid syndrome, which may require additional therapy, alternative anticoagulation, or both. In particular, LA testing may be considered when deciding to place a patient on a direct oral anticoagulant such as rivaroxaban, apixaban, and dabigatran. Meta-analyses of randomized controlled trials with DOACs versus a vitamin K antagonist (e.g. warfarin) found patients randomized to DOACs appear to have an increased risk for arterial thrombosis, without significant difference in risks of venous thromboembolic events or major bleeding.14 Guidelines recommend against use of DOACs in patients with thrombotic triple-positive antiphospholipid antibodies.11,15,16 In these situations, testing may best be coordinated with withdrawal of anticoagulation or alternative anticoagulation less likely to affect the assay results.
In summary, antiphospholipid syndrome diagnosis is challenging, and the level of complication that hemostasis laboratories must deal with has increased in the past few decades with the expanded use of DOACs. Laboratories will best be prepared to handle these challenges by participating in high-quality proficiency testing and expanding their knowledge of these complicating issues. The CAP Hemostasis and Thrombosis Committee strives to support laboratories by providing both of these services.
captodayonline.com
Lupus anticoagulant—proficiency test and preanalytics
Geoffrey Wool, MD, PhD Nicole Dodge Zantek, MD, PhD Marian Rollins-Raval, MD, MPH May 2024—What i...
Sorry, there were no replies found.
Log in to reply.